Occupational Therapy Models
Within the Occupational Therapy profession, models are utilised to support all aspects of the therapy process including assessment, goal setting, intervention and evaluation. Models provide a framework to support a therapist in organising, interpreting and utilising data in a holistic manner. Our therapist utilise a wide range of models (some are briefly described below) as tools to support their clinical judgements.
OPMA
Occupational Performance Model of Australia
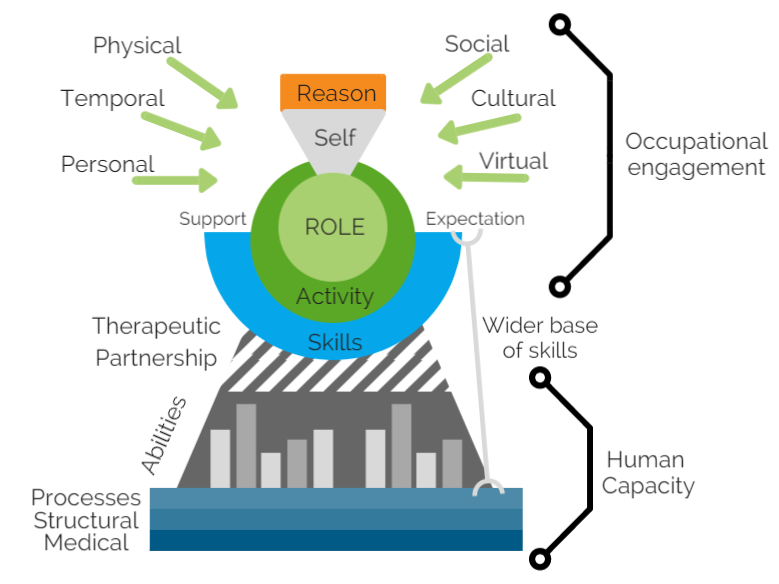
This model was developed by Chris Chapparo and Judy Ranka to “to illustrate the complex network of factors involved in human occupational performance, and the domain of concern of occupational therapy”.
It supports therapists in framing their therapy to achieve occupational performance e.g. “how are leisure activities being impacted by interpersonal factors?”. The complexity of these factors and their interactions are illustrated within the model by interlocking lines (see image).
MOHO
Model of Human Occupation
The MOHO was developed to support therapists in addressing factors beyond motor, cognitive and sensory domains e.g. physical and social environments, sense of meaning in occupations etc. On a personal level it considers
Volition: observes motivation for occupation
Habituation: observes the process of organising actions into habits and roles
Performance capacity: observes underlying physical and mental abilities in relation to the task
From an environmental perspective, the MOHO considers not only physical space, but includes aspects of culture, political and economic features.
In considering these factors, the MOHO provides insight into occupational challenges through the lens of volition, habituation, performance capacity and the environment in, which occupation occurs.
THE KAWA Model
This model offers a client-centered model, where client is the supported to determine what is meaningful across four domains through the metaphor of a river as “life’s journey”:
life and overall occupations (river)
environments / contexts, social and physical (river banks)
circumstances that block life flow and create challenges (rocks)
personal resources that can be barriers or facilitators (driftwood)
From this perspective, Occupational Therapists, serve to support clients in uncovering what is important to their lives and how they can work together to achieve their goals.
Further reading
OPMA: http://www.occupationalperformance.com/
MOHO: https://www.moho.uic.edu/default.aspx
KAWA: http://www.kawamodel.com/v1/